The following is a guest post by Marc Mitchell, Founder and President of D-tree International.
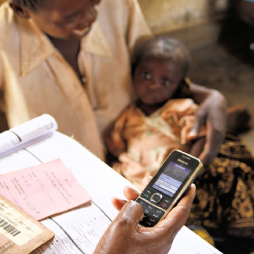
It is time for us to get past the proof of concept stage for mHealth. The concept has been proven. We now have evidence that mobile phones in the hands of a health worker can lead to more accurate diagnosis and treatment of acute problems such as pneumonia and dehydration. Diagnostic tests linked to a phone can improve identification of malaria. Reminders and alerts can help patients remember take their drugs at home. We can reduce the number of stock outs of drugs in a health facility. Community health workers (CHW) can do more with mobile phone support and supervisors can know what they are doing. We have seen a great quantity and quality of health knowledge through broadcast messages and social media to adolescents, mothers, and patients with chronic disease. People can monitor their diet, blood pressure, heart rhythm, breathing, and exercise while sitting at home. Better client knowledge, better provider competence and better systems management lead to better efficiency, higher quality and better health outcomes.
The question now is: where is mHealth going? What will be the shape of mHealth 2.0? Of course, “it’s difficult to make predictions, especially about the future.” (A quote often but incorrectly attributed to Yogi Berra and Nils Bohr. More info). But I think that the future of mHealth can be predicted since most of the components are either already developed or in late stage development. So here is what I see for mHealth 2.0.
 The phone will be the center of diagnostics at home and at all levels of health facilities. Some of you will know about the Qualcomm Tricorder X prize. Ten million dollars for a phone-based device that can diagnose anemia, infections, stroke, lung disease, and a variety of other conditions. But the trick is that most of these diagnostic tests exist today, just not through a mobile device. Each is a standalone device, available for use in the doctor’s office. What is being asked in the competition is to modify the technology so it can use the processing and sensing capability of the phone to accurately make these diagnoses. But this is only the beginning. Within 10 years we will have a mobile phone that can accurately diagnose almost all conditions, using the camera, microphone, and touch screen for inputs with perhaps one or two other wirelessly-linked (think Bluetooth but one that actually works) inputs for things like cardiograms, encephalograms or analysis of blood. This is a modern-day conception of the original tricorder of Star Trek. No limits, it told you what was wrong and how to fix it. Soon to be in the hands of every health worker worldwide.
The phone will be the center of diagnostics at home and at all levels of health facilities. Some of you will know about the Qualcomm Tricorder X prize. Ten million dollars for a phone-based device that can diagnose anemia, infections, stroke, lung disease, and a variety of other conditions. But the trick is that most of these diagnostic tests exist today, just not through a mobile device. Each is a standalone device, available for use in the doctor’s office. What is being asked in the competition is to modify the technology so it can use the processing and sensing capability of the phone to accurately make these diagnoses. But this is only the beginning. Within 10 years we will have a mobile phone that can accurately diagnose almost all conditions, using the camera, microphone, and touch screen for inputs with perhaps one or two other wirelessly-linked (think Bluetooth but one that actually works) inputs for things like cardiograms, encephalograms or analysis of blood. This is a modern-day conception of the original tricorder of Star Trek. No limits, it told you what was wrong and how to fix it. Soon to be in the hands of every health worker worldwide.
But now let’s consider how would we train Dr. McCoy [1] to use this tricorder. Since the tricorder knows which sensing device to use and which test to run, the training would not need to include this. All those years of learning anatomy, physiology, and pharmacology would be unnecessary. What Dr. McCoy needs to know is how to use the machine correctly and how to do procedures that cannot be done by a phone. I wouldn’t expect a phone to remove your appendix, although of course a robot could.
In low income countries, a community health worker would have a tricorder that could diagnose pneumonia, dehydration, malaria and meningitis and tell the CHW what drug to use and when to refer the patient. But the CHW needs to know how to examine a child or how to collect blood for a test. So the training would focus on these skills related to the use of the machine. It might also focus on how to counsel someone with questions about health or about how to take their medicine or nutrition. And knowing the CHW will have a phone in his/her hand also means that we can send periodic updates about new treatments or new diagnostics. Or perhaps the CHW needs to refresh her knowledge of the skills she learned in school. We can send short training videos to the CHW that are based on the original training material and we can have additional information available to the CHW if she wants to know more.
Now imagine a world in which every health worker has a mobile device that does diagnostics like a tricorder. But because it is a phone, the record of what is done at each visit can be documented and analyzed. This is the basis of an electronic patient record so that we can track a patient across multiple visits, keeping track of weight gain or loss, progress during pregnancy, immunizations, or control of a chronic disease. This record is kept on the phone but also synchronized with a cloud-based database enabling records to be transferred from one facility to another when a patient is referred or goes to multiple sites for different types of treatment.
Imagine an example of a pregnant woman on treatment for TB.. She gets followed for TB in one clinic, while her pregnancy is followed in another. She needs a common record so that the staff in each clinic know about what is happening in the other. No problem. Or she visits her mother to have the baby in her home district. Also no problem. This is the value of an electronic patient record. But the record can also be used for other things. By look at patterns of diagnosis we can use it for surveillance. Perhaps there is an outbreak of diarrhea in one region, or an increase in cases of malaria. We can look at diagnosis by provider and find that one provider diagnoses every patient with hypertension. Perhaps the health worker could use some instruction (remotely of course) on hypertension. Or perhaps there is actually an epidemic of hypertension in one area (however unlikely this seems).
In any case, by having the records of each clinical interaction we can know what the health worker is doing, what are the patterns of disease, what are the utilization patterns of drugs. And by using the data we can help supervise the health worker, improve drug logistics and plan resources. Real-time comprehensive data in an easy-to-use format creates an information link across the entire health system improving efficiency and quality of care.
 Finally, imagine too that patients have access to this information – their own patient record. Messages tailored to them about pregnancy, about disease, about care, about their next scheduled appointment. All of this is currently being done, but only in a few places and only one piece at a time. Soon, however, patients will receive information they want in a format that they like. Can I get pregnant from kissing someone? Can I get AIDS from kissing someone? Where is the nearest health facility that can diagnose the cause of my weight loss? Individualized access to information is one of the hallmarks of the internet. Individualized access to health information will be one of the hallmarks of mHealth 2.0.
Finally, imagine too that patients have access to this information – their own patient record. Messages tailored to them about pregnancy, about disease, about care, about their next scheduled appointment. All of this is currently being done, but only in a few places and only one piece at a time. Soon, however, patients will receive information they want in a format that they like. Can I get pregnant from kissing someone? Can I get AIDS from kissing someone? Where is the nearest health facility that can diagnose the cause of my weight loss? Individualized access to information is one of the hallmarks of the internet. Individualized access to health information will be one of the hallmarks of mHealth 2.0.
For those with a smart phone, (which will soon be the only kind of phone – do you really want a stupid phone?) apps will help you with your diet, with your kid’s health needs, with your ability to keep track of drugs you take (or those that your parent or child takes), and with your next appointment. If you need to pay for a clinic visit or a drug or transportation, you will use mobile banking like M-PESA in Kenya and Tanzania. Need to schedule an appointment? Text this number. Want to check if a drug is counterfeit? Text this number. Want to complain about a health worker? Text this number (toll free).
mHealth 1.0 was about technology. mHealth 2.0 is about linkages. Linking clients or patients to knowledge. Linking diagnostics to treatment. Linking health workers to each other. Linking data to action. In making these linkages, mHealth 2.0 will create a new kind of health system — one that works. Or at least one that has the potential to work. Will mHealth 2.0 cure the many problems of health systems today? Obviously not. Only people can make things work. But we now have a tool that uses existing infrastructure to do things that we could never do before. And with that tool we will see health workers who are more competent, patients who are more knowledgeable and systems that are more efficient. That is a good start.
[1] Leonard H. McCoy, was chief medical officer of the USS Enterprise in Star Trek
Photos: Courtesy of D-tree International.